Anders Widmark1,2, Eva Godske Friberg1
- NRPA, Norway
- Gjoevik University College, Norway
Note: This article has already been published in Radiation Protection Dosimetry. Oxford University Press Rightlinks licence 2756401364488
Introduction
The risk for deterministic effects is a potential problem in interventional radiology, and especially when the procedures are performed outside a Radiology department [1]. Cardiology departments often perform advanced interventional procedures, but the competence and attitudes towards radiation protection can sometimes be absent [2]. The International Atomic Energy Agency has also recently highlighted the importance of radiation protection and competence in interventional cardiology, and has also arranged several courses and produced training material for radiation protection in cardiology [3]. The Norwegian Radiation Protection Authority (NRPA) was contacted by a Cardiology department with a request for assistance with dose measurements. The department performed bi-ventricular pacemaker (BVP) implants, which is a technically complicated treatment for patients with severe heart insufficiency. The department had recognized a suspicious radiation burn on a patient, three weeks after a BVP procedure. The particular patient had undergone two BVP implants and the lesion had the size of a palm. The lesion was situated on the back of the patient and was recognized as radiation dermatitis. The aim of this work was to illustrate that the patients skin dose are very dependent of the equipment used and the operators working technique and that skills in radiation protection can significantly reduce the skin dose.
Material and method
To assist the Cardiology department with skin dose measurements the NRPA prepared sets of thermoluminescense dosemeters (TLD’s) (LiF:Mg,Ti, Harshaw TLD-100 chips; Harshaw/Bicron, Solon, Ohio, USA), each containing 10 TLD’s. The TLD’s in each set was arranged in a star pattern for covering a large area of the patients back. The TLD arrays were sent to the Cardiological department by post, with instructions to place them on the patients back where the most likely peak-dose would occur. It was corrected for the background radiation by control TLD’s following the postal sending. Dose measurements were performed on eight subsequent patients and the TLD’s were afterwards read at the NRPA laboratory. After the eight initial dose measurements, a site audit was performed at the Cardiological department. Characteristics for the equipment were registered and the working technique and general skills in radiation protection during a BVP procedure was observed. Based on the findings during the audit, a short meeting were held with the participating staff, where the working technique was discussed. After the audit, new sets of TLD’s were distributed and dose measurements were performed on six new patients.
Results
The X-ray equipment was a Siemens Multiscope (1989) with a 40 cm diameter image intensifier (II). The equipment was intended for abdominal angiography and was considered not suited for coronary procedures, due to the large II, poor dose reduction options and lack of dose monitoring device. The large II made it also difficult to use optimal short II to skin distance, since the II came in conflict with the patients head. During the procedure it was a prerequisite to use magnification technique with a 28 cm diameter II entrance field to get a sufficient image quality. The equipment did not have any options for pulsed fluoroscopy or last-image hold. However, there was a possibility for extra filtering of the X-ray beam, but this option was not used. The dose rate was not adjusted by the cardiologists to the actual image quality needs during the different steps of the procedure, resulting in a high dose rate throughout the procedure. The audit also gave an impression that it was an over-use of fluoroscopy. During the image acquisitions, the acquisitions were started at the same time as the contrast injector started. This results in unnecessary radiation, because of wasted images during the time it takes before the contrast medium reaches the heart. All together, the working technique was fare from optimized with no focus on radiation protection.
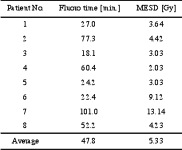
The average maximum entrance surface dose (MESD) for the first eight patients was 5.3 +3.8 Gy, ranging from 2.03 to 13.14 Gy. The fluoroscopy time varied from 18.1 to 101 minutes, with an average of 47.8 + 30.2 min (table 1).
Table 1. Fluoroscopy time and maximum entrance surface dose (MESD) for the initial eight patients
During the meeting, directly after the audit procedure, the following “Do’s” and “Don’ts” were given as a first attempt to reduce the doses:
- Don’t over-use the fluoroscopy.
- Do adjust the image quality to the actual needs during the different steps in the procedure.
- Don’t start the image acquisition before the contrast medium has reached the heart.
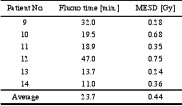
The TLD measurements on the six consecutive patients following the educational meeting showed a significant skin dose reduction with an average MESD of 0.44 +0.2 Gy, ranging from 0.24 to 0.75, which is less than 10 % of the previous average. The average fluoroscopy time was also decreased from 47.8 to 23.7 + 13.5 min, which is a 50 % reduction (table 2). All these six patients were below the threshold for deterministic effects [4][5].
Table 2. Fluoroscopy time and maximum entrance surface dose (MESD) for the six patients following the educational meeting.
Discussion and conclusion
The patient doses during BVP procedures can easily reach thresholds for deterministic effects. The BVP procedures in this department were performed on suboptimal equipment, with poor reduction possibilities and the lack of dose monitoring device. The use of this equipment underlines the lack of competence in radiation protection and understanding of optimal use of the equipment.
The maximum skin dose of 5.3 Gy found in this case are not surprisingly much higher that those reported by others. Taylor and Selzman reported values of 1,6 +1,8 Gy and 36.4 +16.5 min for average MESD and fluoroscopy time respectively during BVP [6]. The reported fluoroscopy time is similar to the one found for the eight initial patients, indicating that the excess dose are due to a higher use of cine together with short source to skin distance, high dose rate and use of magnification. Also the maximum skin dose measured in this study are likely to be underestimated, since dose measurements using TLD arrays often fail to capture the hot-spots given by overlaying radiation fields. Another factor influencing the accuracy of the measured MESD is the subjective placement of the TLDs by the operators, with no control by the NRPA. Interventional procedures are also dynamic in nature and can vary from patient to patient for the same type of procedure. To increase the accuracy of the dose measurements radiochromic film should have been used, but in this case the goal was to assist the cardiology department with easy measurements to identify the dose level.
The initial eight measured patient doses were all above the threshold for deterministic effects. The threshold for an early transient erythema is considered to be 2 Gy and the patient with the highest dose, which was 13.1 Gy, was above the threshold for severe effects like dermal atrophy and teleangiectasis [4][5]. When the cardiologist realised that they delivered doses capable of giving deterministic effects on their patients, they become more aware on radiation protection and interested in learning a more appropriate use of the equipment.
After the audit and the educational meeting, where the three “Do’s” and “Don’ts” were given, the average MESD for the six monitored patients were 0.44 +0.2 Gy. This is below the values reported by Taylor and Selzman and also far below the threshold for deterministic effects. The 50 % decrease in fluoroscopy time gave a significant contribution to the decrease in skin dose. Additional significant factors to the decrease in skin dose were to start the image acquisition when the contrast media reaches the heart and to adjust the image quality to the actual needs during the different steps in the BVP procedure. The enormous dose reduction achieved by proper use of the equipment also motivated for a change in attitudes towards radiation protection of the patients. To fully optimize the procedure, with respect to patient doses, much more efforts have to be put in the education of the operators and to start using equipment dedicated for coronary procedures.
Further optimization on this particular equipment should comprise a reduction of the acquisition frame rate and use of the optional extra filtering to reduce the skin doses [7][8]. Use of extra filtration has to be balanced with the decrease in image contrast. The revealed conditions in this case were not in compliance with the Norwegian radiation protection regulation, which requires that interventional procedures shall be performed on dedicated equipment and performed by skilled operators. Based on this, the department were given corrective actions e.g. to change the equipment or use another interventional suite, implement an educational program for all involved staff and to develop procedures for follow-up of patients with skin doses above 2 Gy.
Despite the suboptimal equipment, it was possible to decrease the patient doses significantly, which shows that competence is a key factor in radiation protection.
Education and training is also proposed as a success factor for radiation protection by the International Atomic Energy Agency, International Commission on Radiological Protection and Wagner and Archer [9].
Later inspections in the department, showed a significant improvement in skills and attitudes towards radiation protection. New dedicated equipment had been purchased, comprising dose reduction techniques and dose monitoring device. There was also a more serious focus on education and training, and the department had procedures for follow-up of patients receiving skin doses above 2 Gy.
This case has shown that a few very basic advices on operation technique can give significant results in dose reduction, especially if the user has no previous competence in radiation protection.
References
[1] Food and Drug Administration. Avoidance of serious X-ray induced skin injuries to patients during fluoroscopically guided procedures. Important information for physicians and other health care professionals. FDA, September 9, 1994.
[2] Friberg EG, Widmark A, Solberg M, Wøhni T, Saxebøl G. Not able to distinguish between X-ray tube and image intensifier: fact or fiction? Skills in radiation protection with focus outside radiological departments. Proceedings from 4th International Conference on Education and Training in Radiological Protection. Lisboa, Portugal 8-12 November 2009. ETRAP 2009.
[3] International Atomic Energy Agency, IAEA. Regional training courses on radiation protection in cardiology organized under TC support. Vienna: IAEA, 2009. http://rpop.iaea.org/RPOP/RPoP/Content/AdditionalResources/Training/2_TrainingEvents/Cardiology.htm (15.11.2010)
[4] Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. Journal of Vascular and Interventional Radiology 1994; 5:71-84.
[5] ICRP Publication 85. Avoidance of radiation injuries from medical interventional procedures. Annals of the ICRP. International Commission on Radiological Protection, 2000.
[6] Taylor BJ. and Selzman KA. An evaluation of fluoroscopic times and peak skin doses during radiofrequency catheter ablation and biventricular internal cardioverter defibrillator implant procedures. Health Phys. 96(2):138-43; 2009.
[7] Nicholson R, Tuffee F, Uthappa MC. Skin sparing in Interventional Radiology: The effect of copper filtration. Br. J Radiol 2000: 73:36-42.
[8] Gagne RM, Quinn PW. X-ray spectral considerations in fluoroscopy. In: Balter S and Shope TB (eds.): Physical and Technical Aspects of Angiography and Interventional Radiology: Syllabus for a Categorical Course in Physics. Oak Brook, IL. Radiological Society of North America, 1995, 49-58.
[9] Wagner LK and Archer BR. Minimizing risks from fluoroscopic X rays. 4th ed. Partners in Radiation Management, LTD. Company; 2004.
