Newsletter 30
Carole Rousse (Deputy Head ASN Ionising Radiation and Health Department, France)
Introduction
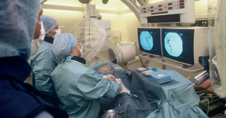
On March 20, 2009, the French Nuclear Safety Authority (ASN) was informed by the Strasbourg Academic Hospitals (HUS) of reports of patients presenting adverse reactions, of unusual intensity, consisting of hair loss over a large surface area and/or cutaneous erythema. These patients received treatment at the Hautepierre Hospital site by means of the same X-ray device used to guide practitioners during treatment of cerebrovascular disease.
ASN carried out a number of inspections on March 23, May 7, and September 29, 2009, so as to analyse the circumstances and causes of the occurrence of these adverse reactions, and to examine the corrective action implemented.
At the same time, the ASN and the French General Directorate for Health [Direction générale de la santé] jointly referred to the French Institute of Radioprotection and Nuclear Safety (IRSN) in order to reconstitute the doses received by the patients and to analyse any potential complications in exposed patients. Follow-up of patients carried out by HUS to date does not reveal any neurological, meningeal or subcutaneous abnormalities, and the cases of alopecia observed have fully regressed. Today, all the cases of alopecia have disappeared.
Results of the investigations
The different investigations and expert appraisals carried out revealed that the device in question did not present any technical faults and that insufficient attention had been given to optimising and monitoring the doses received by the patients. The effects observed are due to the use of a new device and the fact that the conditions relating to use and settings were not optimised, contributed to by inadequate training and organisational failings.
A number of failings were observed, at establishment level, in medical and paramedical personnel training in the knowledge of the devices and in the implementation of a dose-optimisation procedure, and also in the mastery of the maintenance and adjustment process for the device, together with the organisation of medical physics. Furthermore, the investigations evidenced a number of failings in the traceability of the maintenance operations carried out by the manufacturer, in the training provided by the latter for users of the device, and, lastly, in the optimisation of settings carried out during commissioning and maintenance operations. A number of contributing factors related to the device were identified, such as the absence of standardisation of measurable dosimetric quantities, the difficulty in monitoring doses based on the DAP [1], the absence of automatic dosimetric data export from the devices to the databases enabling them to be processed.
Moreover, the DAP levels during treatment of cerebrovascular diseases at the HUS as a whole (Hôpital Civil and Hautepierre) generally appear to be higher than those reported in the majority of the French and international literature reviewed. However, although the literature states that a dose-optimisation margin exists, it seems hard to determine whether these levels and the incidence of effects differ considerably from other French sites, in the absence of available reference systems and reliable local data. It appears likely that the findings observed locally during the investigations are not specific to the HUS.
Action plan implemented by the establishment, and the results obtained
The lessons drawn from analysis of this event enabled the HUS to define and implement a logical and innovative action plan, the aim of which is to identify and reduce the dose levels for all interventional procedures. Owing to this action plan, the HUS is now among those French establishments which follow the most advanced practices in terms of patient radioprotection in the field of interventional radiology.
The corrective action implemented by the HUS involved:
- implementing an optimisation procedure with regard to settings, in connection with the manufacturers,
- modifying the conditions of the devices (reduction in the number of images, selection of an image type requiring less radiation),
- modifying the organisation of the interventions (dedicated operators, intervention of an experienced practitioner from the start of complex procedures),
- automatically collecting the DAP for each procedure,
- systematically consolidating and processing the DAP,
- defining in-house dose reference levels,
- implementing self-assessment of practices, through processing dosimetric data,
- identifying and monitoring patients liable to present iatrogenic effects.
Lastly, the HUS initiated an innovative in vivo dosimetry process. Furthermore, work has begun with the manufacturer to improve the coordination and traceability of maintenance operations together with the possibility of developing a system able to monitor, in real time, skin dose mapping for doses delivered to patients.
The results obtained are significant and demonstrate the relevance of the action plan. This has led to a considerable reduction in the doses delivered to patients, in the region of 40% related to changes in the settings, and in the region of 30 to 50% related to the changes in practices relating to the use of the devices. Owing to these results, the occurrence of adverse reactions is now very rare.
Action relating to the monitoring of dosimetric data, and, in particular, the implementation of in vivo dosimetry, will moreover make it possible to determine more accurately the doses received by patients, which are still poorly evaluated and insufficiently documented.
Experience feedback
In addition to the teaching and corrective action implemented locally by the HUS, this event has given rise to considerable experience feedback for all professionals, and also for manufacturers and personnel responsible for device maintenance.
This event has reiterated the importance of the challenges in terms of dosimetry facing this type of activity, and has shown that the effects it can generate are largely unknown. The current regulatory system is not sufficiently applied or adapted. In particular, the concept of an optimisation procedure, which is a fundamental principle of radioprotection, is not sufficiently known or assimilated in the different departments. Likewise, technical mastery of equipment, radiovigilance and follow-up of complications, which should be at the centre of all procedures aiming for an improvement in practices, are inadequately defined and organised. This event also has demonstrated the existence of considerable margins for progress in terms of dose reduction, without compromising therapeutic efficacy.
Based on this experience feedback, ASN reiterated the regulatory requirements, in a memorandum dated December 11, 2009, and sent a number of recommendations to the heads of interventional vascular neuroradiology departments, together with the general managers of regional and academic hospitals with a view to improving interventional radiology practices.
Furthermore, ASN informed the French Health Products Safety Agency (AFSSAPS) of the lessons drawn from this feedback and the improvements which needed to be made both in terms of relations between the supplier of the device and the user during commissioning, maintenance, and the training provided, together with the ergonomic aspects and settings for devices used in radiology.
Although failings were evidenced locally, this event made it possible to identify a number of weaknesses and courses of action which need to be taken into account at national level. These were brought to the knowledge of the permanent medical radioprotection expert group (GPMED), convened by the ASN in January 2009, so as to draw up recommendations to improve radioprotection among patients and personnel in interventional radiology. The conclusions of this expert group have been taken into account in the ASN Deliberation issue on 5 July 2011 on the improvement of radiation protection in interventional radiology available on the following link: http://www.asn.fr/index.php/Les-actions-de-l-ASN/La-reglementation/Bulletin-Officiel-de-l-ASN/Deliberations-de-l-ASN/Deliberation-n-2011-DL-0018-de-l-ASN-du-14-juin-2011. The medical physicist appears as a key actor of the optimization of doses delivered to the patient.
