Newsletter 28
C. Lefaure
In France there are currently more than 20,000 “Personnes Compétentes en Radioprotection” (PCR)/Radiation Protection Officers (RPO) and other radiation protection partners, such as occupational physicians involved in radiation protection. In the medical, research and non nuclear industry sectors, they can often feel isolated, not given appropriate recognition either within their organisations or by their colleagues, and sometimes struggle to keep up to date in regard to the continuing changes in regulations which have evolved significantly in recent years.
In order to address some of these concerns, a number of networks have recently been established at regional levels to provide a forum to share experiences and to learn from both each other and also from experts such as regulatory bodies and commercial companies. The desire to establish these networks began several years ago, but real progress was made during 2009 and 2010. At the beginning of 2011, eight networks have now been set up, covering approximately half of the 22 regions in France. One thousand individuals now participate in these networks, which continue to increase both in size and in the range of activities carried out. Typical activities include the holding of seminars and the creation of working groups, the establishment of web forums, sector specific training initiatives and the publication of newsletters. Seven of the networks are open to participants from all sectors (medical, research, industry) while the eight one is dedicated solely to participants in the medical sector.
In establishing these networks, the participants now feel that there is at last a forum in which their concerns can be addressed and their status among their colleagues, and within their organisations, is now better recognised. In recognition of the importance of participation at seminars, one of the networks now provides an official “continuing training certificate” to all attendees. It is interesting to note that this network is the only one to regularly receive participants from the industrial sector. Three of the networks also have the support of an important public institution, such as a regional hospital or a university. In addition to promoting and facilitating the exchange of information between members, the networks also play an invaluable role in providing data and feedback on topics to the IAEA and other bodies on issues such as incidents for the RELIR OTHEA system, data on doses and number of procedures in interventional cardiology services and in industrial radiography companies. This is a great benefit to the IAEA, and other organisation, which would otherwise have difficulties collecting such data.
The active participation in such networks is now recognised by the French regulatory bodies (ASN and Ministry of Labour) as being extremely important and consideration is being given to making such participation a positive criterion for the renewal of the PCR certification. Furthermore, the competent authorities have also discussed the assistance they could bring to the creation of new networks and ensuring the life of the existing ones (further information can be found on the ASN website). The next step in this initiative is for these networks to be coordinated at a national level bringing together all the pilots of the regional networks.
In light of this recognition and support, further development of the current networks and the appearance of new networks to cover all parts of France are anticipated. However, it may not be possible to include each and every one of the 20000 players currently involved in radiation protection in these networks, particularly those outside the medical sector. The existence of Web forums will help to reach some of them, but Imagination, the key to all of these networks, will have to find new ways to involving everyone in the years to come.
L. Garbarino, M. Calimero
ARPAL, Environmental Protection Agency of Liguria - Italy
Description of the incident
In summer 2010 in the port of Genoa, routine radiation monitoring on incoming metallic objects detected an unexpected peak of gamma emissions coming from a container which had arrived from the United Arab Emirates. The radiation levels detected were significantly above background radiation levels. Immediately after the discovery, a Safety Plan was activated involving specialists from the Regional Environmental Agency (ARPAL) and fire fighters, with overall coordination of the plan by the Prefecture of Genoa. A precautionary no entry or exclusion zone was established at a distance of 200 m from the container; in spite of this, at the edge of the exclusion zone an environmental dose rate equivalent of 250 nSv/h could be measured, which is approximately four times higher than background levels. Measurements carried out on the container included gamma spectrometry, dose measurements and wipe testing, and the source of the radiation was identified as 60Co. Fortunately, no environmental contamination had occurred. At present, the container is still under judicial attachment.
The maximum values of environmental dose rate equivalent measured were:
- 36 mSv/h, at a distance of 0.1 m from one of the long sides of the container;
- 15 µSv/h, on the other long side of the container;
- 40 µSv/h and 75 µSv/h on the short sides of the container.

Photo 1. The container with the 60Co source on the wharf of the port of Genoa
Radiological Consequences
It is possible that workers on both ships and on the wharf may have been significantly exposed prior to the detection of the source. Hypothetical doses to these workers were estimated for a worst case scenario which assumed long exposure times, minimum distances between the container and the workers and no in-situ shielding between the source and the workers. The results of this assessment suggested that the maximum estimated effective dose to these workers would not have exceeded 1 mSv.
Lessons Learned
In order to avoid future exposure of workers to sources of ionising radiation from shipments of metallic materials, it would be advisable to:
- require sellers to provide certificates of the results of radiation monitoring of the containers;
- install radiation monitors on cranes, to provide for real time monitoring of containers during ship loading and unloading;
- provide the front line workers handing the containers with personal dosimeters.
G. Frasch
Federal Office for Radiation Protection - BfS, Germany
In Germany, about 2,500 workers are registered within the occupational category Industrial Radiography in the German Radiation Protection Register of the Federal Office for Radiation Protection (BfS). Industrial radiographers traditionally belong to one of the critical groups among radiation exposed workers. Their average annual personal doses are approximately in line with those from specific groups in the nuclear sector, nuclear medicine or interventional radiography in the medical sector and last but not least air craft crews.
The working conditions for workers in mobile industrial radiography are often exceptional. Their dosemeter evaluations frequently show smaller doses of typically one or two millisievert every month and occasionally higher doses from single incidents which, when summed, may occasionally lead to a dose limit being exceeded. In spite of the sometimes adverse working environment in on-site industrial radiography, the radiation exposure in this sector decreased substantially from 1998 to 2009 (Figure 1). It is interesting to study the change in the dose distributions over the years and to see how the fraction of workers in the different dose intervals changed and reached dose ranges which are seemingly hard to further reduce.
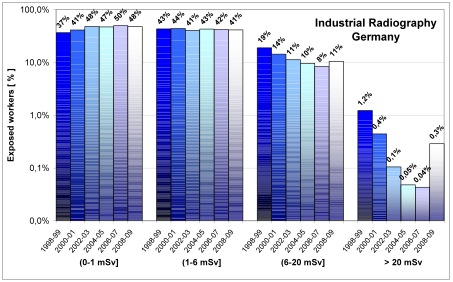
Figure 1. Change of frequency distribution of annual doses from 1998 to 2009
Cases > 20 mSv/yr: the systematic reduction in the number of workers exceeding the dose limit seems to have reached its optimum at a value below 0.5% of the measurably exposed workers. These remaining cases with overexposures seem to occur stochastically. The pattern of their monthly doses usually consists of numerous small dose values over the year, interrupted by one or two higher dose values that result in the dose limit being exceeded. The fact that there are now relatively few cases of the limits being exceeded, together with the observed characteristic pattern of monthly doses, would suggest that they cannot be avoided by applying generic ALARA measures; instead they should be addressed by specific analyses of incidents.
Cases between 6 - 20 mSv/yr: Optimisation can also be stated below the dose limit, in particular within the dose range of 6 - 20 mSv. During the course of the last decade about 10% of all measurably exposed workers remained within this dose range and it appears difficult to further reduce this value.
Cases between 1 - 6 mSv/yr: slightly more than 40% of the exposed radiographers stay relatively constant in this group.
Cases ≤ 1 mSv/yr: nowadays approximately half of all workers in this sector receive annual doses less than millisievert per year. This group necessarily increased as workers shifted from intervals with higher doses towards lower ones.
Up until 2003 there was a substantial decrease in the number of exposures that were received. In particular, the change in the intervals above 6 mSv indicates the results of a successful optimisation process. As the relative numbers remained comparably stable during the consecutive six years, it seems that optimization has lead to a level of exposure which cannot be further reduced.
By studying the changes in dose distributions it can be clearly seen the level at which systematic dose reduction has reached a level of exposure where stochastic processes (statistics) dominate. It also illustrates that a stage will occur where a generic technical and organisational measures approach to optimisation may no longer be effective and suggests that ALARA measures would be better focused on stochastically occurring single cases.
These stochastically occurring cases are probably less induced by insufficient technical protection measures; the reason lies more likely in the lack of ALARA culture, i.e. in the mind set of the workers and their management. The ALARA awareness of the workers gains importance when working on site and in absence of the direct supervision of a radiation protection officer (RPO). This ALARA awareness can be raised through briefings before and debriefings after the concrete exposure situation by the RPO. It is useful to utilize the information that is delivered from film dosemeters. Besides the individual dose, film dosemeters provide quite useful additional indicator information: together with the dose value and the exposure direction, the film can reveal specific exposure circumstances or operational mishaps that lead to exposure. Wrong handling of the film dosemeter can also be identified (Figure 2).
About 7% of all industrial radiographers are irradiated from the side and about 3% from behind. Both numbers are twice as high as the respective rates among all radiation workers and the rates remained relatively constant over the years. The analyses of the exposure direction may reveal operational mishaps or inattentiveness that lead to exposure.
Incorrect handling of the film dosemeter can also be an interesting indicator information: the rate of industrial radiographers who insert the film incorrectly into the dosemeter is seven times higher than the rate among all radiation workers. This indicates that there could be concerns regarding a group-specific lack of knowledge if not negligence in this sector rather than occasional inattention by inidvidual workers. In both cases, information about irregular dosemeter handling can be used for individual feedback in order to enhance the level of protection by raising ALARA awareness.
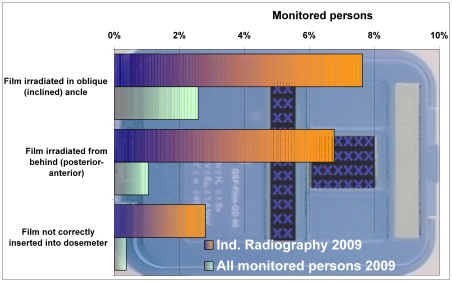
Figure 2. Mishaps or inattentiveness? What film dosemeters reveal.
S. Christofides1, R. Padovani2, W. Van der Putten3, A. Torresin4, P. Allisy-Roberts5, C.J. Carvana6, P. Sharp7, K-U. Kash8
1 Medical Physics Department, Nicosia General Hospital, Nicosia, Cyprus
2 SO di Fisica Sanitaria, Ospedale S. Maria della Misericordia, Udine, Italy
3 Department of Medical Physics and Bioengineering, Galway University Hospitals, Galway, Ireland
4 Medical Physics Dept, Azienda Ospedale Niguarda, Milano, Italy
5 Ionizing Radiation Department, International Bureau of Weights and Measures (BIPM), Sèvres, France
6 Biomedical Physics, Imaging and Devices. Radiation Protection, Quality Control of Imaging Devices, Faculty of Health Sciences, University of Malta, Msida, Malta
7 Bio-Medical Physics & Bio-Engineering, University of Aberdeen & Grampian Hospitals NHS Trust, Aberdeen, UK
8 University of Applied Sciences (BHT), Berlin, Germany
Abstract
As low as reasonably achievable (ALARA) has long been associated with ionising radiation and ALARA is a key to ensuring the safe and appropriate use of medical radiation in healthcare. This article describes a Medical ALARA Culture as part of the wider safety culture in the healthcare environment. To illustrate this, the various hazards that are present when caring for patients are briefly discussed to put the hazards associated with medical radiation use into context. It is emphasised that within the context of the Medical ALARA culture, the requirement of ensuring the adequate diagnosis and optimal treatment of the patient is paramount.
Introduction
The ultimate goal of any healthcare facility is to deliver high quality, safe and patient oriented medical care. We all know that this ultimate goal can be very difficult to fulfil for each and every patient as there is a large variety of hazards that may hinder its fulfilment. In order to appreciate the importance of ionising radiation as used for healthcare in both diagnosis and therapy, and also its relative contribution to the overall hazards in the healthcare environment, the types of hazards present as well as the adverse events they may invoke are presented in this article. This is to emphasise the relevance of radiation protection as an indispensable component of safety culture and the increasing need over the last few years to develop a Medical ALARA Culture within the healthcare environment.
Hazards within the Healthcare Environment
There are very many hazards associated with a healthcare environment. For example, the Occupational Safety and Health Administration (OSHA) of the United States of America classified the potential hazards in a hospital into a number of categories [1]. These hazards can affect the patient and the staff as well as other persons present within the hospital and are listed here in a risk-related order. Each of these hazards can also be the underlying cause of a medical error and consequently, the concept of minimising the hazard can also reduce overall risks.
Biological
Biological hazards are the infectious/biological agents, such as bacteria, viruses, fungi, or parasites that may be transmitted by contact with infected patients or contaminated body secretions/fluids. Common examples include the Human Immunodeficiency Virus (HIV), vancomycin resistant enterococcus (VRE), methicillin resistant staphylococcus aureus (MRSA), hepatitis B virus, hepatitis C virus and tuberculosis.
Chemical
Chemical hazards are the chemicals that are potentially toxic or irritating to the body system, including medications, solutions, and gases. Examples include ethylene oxide, formaldehyde, glutaraldehyde, waste anaesthetic gases, hazardous drugs such as cytotoxic agents and pentamidine ribavirin.
Physical
Physical hazards are the agents within the work environment that can cause tissue trauma. Examples include ionising radiation including radiation beams and unsealed radionuclide sources, lasers, ultraviolet light, noise, electricity, extreme temperatures and also workplace violence.
Psychological
Psychological hazards are defined as the factors and situations encountered or associated with the job or work environment that create or potentiate stress, emotional strain, and/or other interpersonal problems. Examples found in the health care environment include stress, workplace violence, shift work, inadequate staffing, heavy workload and increased patient acuity.
Environmental, Mechanical/Biomechanical
This group concerns the factors encountered in the work environment that cause or potentiate accidents, injuries, strain, or discomfort. Examples include tripping hazards, unsafe/unguarded equipment, air quality, slippery floors, confined spaces, cluttered or obstructed work areas/passageways, forceful exertions, awkward postures, localized contact stresses, vibration, temperature extremes, repetitive/prolonged motions or activities, lifting and moving patients.
From the list above, one may conclude that the hospital is, potentially, a highly dangerous environment in which to be treated, to work, or simply to be present. Indeed, ionising radiation is only one of this long list of hazards and sometimes, when the radiation risks are carefully controlled, one can understand why some hospital managers have a higher priority concerning the control of some of the other, even more deadly, hazards. However, managers in hospitals have the responsibility to ensure that all these hazards are eliminated or at least minimised as much as possible taking into account the required outcome the safe and complete healthcare of the patient.
Quality and Safety Culture
Many models and systems for quality and risk management have been developed and implemented in an effort to mitigate the hazards and errors within the healthcare environment so as to improve the safety of the patients and staff. These have proved to be effective within individual departments but do not necessarily present the desired effect in improving the safety of the patient within the healthcare facility as a whole. Successful patient treatment depends on the collective effort of many departments, in providing for example, laboratory test results, diagnostic imaging examinations, surgical procedures, radiotherapy etc. All departments must work together with this common aim.
More recently, Quality Management systems have been implemented that do involve the whole healthcare facility based on Integrated Risk Management Systems [2]. These systems consist of a large number of parts and use tools that need to be implemented effectively. However, such systems alone cannot be effective if the healthcare facility employees do not adopt a Quality and Safety Culture [3] before such systems are implemented.
The analysis of the above systems is beyond the realm of the present article whose focus is that the use of ionising radiation is a physical agent that comes with associated hazards and should be subject to the Medical ALARA culture. The management of the risks (and even potential errors) associated with ionising radiation needs to be implemented as an integral component of the whole healthcare facility Quality Management System.
Medical ALARA Culture
There is, as yet, no universally agreed definition of an ALARA culture, despite the wide acceptance of the need for such a culture [3]. However, the European ALARA Network has proposed a definition of the ALARA culture as an approach to the Radiation Protection Culture [4].
To understand how such an ALARA culture can be developed within the healthcare environment as a Medical ALARA culture, we need first to recall the basic principles of radiation protection.
It is commonly known that to be acceptable, radiation use must fulfil the following basic principles:
- Principle of justification
The benefits of using radiation must outweigh the risks. - Principle of optimisation
Radiation exposure from the use of radiation must be kept as low as reasonably achievable (ALARA), consonant with the desired medical outcome. - Principle of limitation
Obviously, the exposure of radiation workers and other individual members of the public (bystanders) must not exceed the relevant dose limits but it must be recognised that the principle of limitation does not apply to patients or their personal comforters and carers undergoing the medical exposure.
In Europe, it is a legal obligation to ensure all the above basic principles are fulfilled for any new installation or procedure using ionising radiation to operate safely [5] within the healthcare environment [6].
A discussion follows on how the basic principles, are applied in the healthcare environment. The discussion starts from the principle of justification, then optimisation and finally limitation, responding to the special situation faced in the healthcare environment that revolves around patients.
Principle of justification for medical radiation exposures
Justification is the process of ensuring that the benefits from an activity outweigh the harm resulting from that activity. In terms of medical radiation exposures, there are three levels of justification, the first of which results from the decision that medical exposures (in general) do more good than harm, and this is usually taken for granted.
The second level of justification (often called generic justification) is concerned with whether a specified procedure will be beneficial or not for a given subset of patients and will not involve unacceptable risk to the health workers involved in the procedure. Consideration also needs to be given to possible exposures of bystanders, i.e. members of the public who may be inadvertently exposed because of the procedure, and also to the patients comforters and carers who are willingly and knowingly exposed, having been informed of the potential doses and associated risks. Referral criteria [7] are an important tool in the practical implementation of the principles of second level justification in diagnostic imaging.
Justification at the third level is justification of the individual exposure. This level of justification must be carried out through consultation between the radiological medical practitioner and the referring medical practitioner, and may go beyond the requirements for the second level of justification.
To illustrate this, one can consider the case of a simple screening / diagnostic procedure. Mammography is widely accepted as an essential tool to screen for and characterize breast cancer. In the case of screening the second level justification process may entail just a confirmation that the person to be screened fits into the patient group for whom the procedure is deemed justified i.e. is female and is in the recognised age range for the benefit to outweigh the risk of cancer induction (assuming that the doses are properly controlled). In addition, the person justifying the examination must be satisfied that the information requested is not already available because the patient has recently undergone the same examination elsewhere, and so a further radiation exposure can be avoided (Medical ALARA Culture).
Third level justification at the individual level may be illustrated as follows. Consider a female of age lower than the recognised age range for the benefit to outweigh the risk of cancer induction but who has a history of breast cancer in the family. In this case although the procedure is not justified at the second level it is so at the third level.
Principle of optimisation
Optimisation implies that, once the procedure has been justified, every effort is taken to optimise the exposure for the procedure. For example, the equipment emitting ionising radiation is calibrated and maintained so as to provide the required end-product by using the minimum radiation possible to achieve the medical aim. This will involve acceptance testing by the provider of the equipment and confirmation by a Medical Physicist who will usually commission the facility prior to its use on patients. At this stage, specific optimisation procedures may have to be developed to find the best possible operational parameters. The result of these activities is equipment that is optimised to produce the required output for each diagnostic or therapeutic procedure. The values for each performance indicator obtained during the acceptance testing and the commissioning of the equipment are used as the base values for the periodic routine quality control tests. The cycle of quality control tests, preventive maintenance, corrective maintenance and finally replacement of the equipment is continuous through a defined periodic programme throughout the useful life of the facility.
In the healthcare environment, we then need to optimise the positioning of each individual patient and to refine the exposure parameters based on the patients anatomy, age and weight so as to keep the dose ALARA and at the same time achieve the required diagnostic or therapeutic outcome of the procedure. An effective quality assurance tool for confirming that diagnostic doses are indeed ALARA for the patient requires procedures for recording doses to standard sized patients, or alternatively, a large amount of patient dose data automatically collected from digital images. These data can then be compared with national, or international diagnostic reference levels. However, this is only effective if the images are of adequate quality to enable an accurate diagnosis. In therapy, even more care has to be taken to ensure that the prescribed doses are delivered correctly to the tumour with the surrounding tissue receiving doses that are ALARA; this is not easy to achieve in the field of radionuclide therapy using unsealed sources in the body.
The recent evidence that exposure to low doses of radiation, such as those received by patients during radiodiagnostic procedures, increases the risk for cardiovascular diseases [8] have made it imperative that awareness campaigns take place in all healthcare facilities to highlight the importance of optimisation for each individual patient exposure. The emerging evidence of increased lifetime attributable risk (LAR) of cancer onset from low doses [9, 10] has also contributed to the above need. The practical aspects of ALARA include limiting the exposure only to the part of the patients body that we need to examine or treat, by protecting all the other body parts where practicable but without negating the desired medical outcome.
With the recent increasing awareness of the importance of radiation protection and because higher quality images often entail higher doses, a paradigm shift can be observed in radiology in particular from the principle of image quality as good as possible to image as good as needed [11]. This constitutes evidence that optimisation is now being interpreted better within a Medical ALARA Culture.
Of course, when a new facility is planned, the optimisation process, with regard to workers and the general public starts at the planning stage. To ensure the maximum protection the facility should be designed to offer the necessary radiation shielding according to the occupancy of the areas around, above and below the installation to keep doses ALARA.
Principle of limitation
It is a legal obligation to restrict the doses resulting from the radiation exposure of workers, apprentices, students and members of the public (other than patients and their comforters and carers) to ionising radiation to below the limits stipulated in legislation [5].
Here we need to provide shielding to the users and other medical workers that need to be in the room during the use of ionising radiation (this is particularly important for interventional procedures). The emerging evidence that interventional radiologists could suffer from radiation-induced cataracts [12] indicates that greater care is required for the more radiosensitive organs.
It is important to note that the only situation in which ionising radiation is deliberately used to expose humans, above accepted radiation levels that are known to cause biological effects, is in the healthcare environment. For medical reasons there can be no legal limit to the dose a patient can receive, and as a consequence the dose from the procedure to each individual patient must be justified and optimised. This is the basis of the Medical ALARA culture.
Discussion and Conclusions
To achieve a Medical ALARA Culture, it is important to establish a safety-based attitude in every individual healthcare worker so that radiation protection and radiation accident prevention are regarded as a routine part of everyday duty. This objective is primarily achieved by education and training, by encouraging a questioning and learning attitude, and also by a positive and cooperative attitude from management. The national authorities can have a significant role and major impact in achieving this by providing adequate surveillance and advice.
A feeling of responsibility can only be achieved if the healthcare professionals are themselves involved in the formulation of the rules and regulations that are necessary, so that they can thus recognise and accept that these are a support to and not a hindrance in their daily work. For an effective Medical ALARA Culture, the efforts of various categories of personnel engaged in the medical use of ionising radiation must be coordinated and integrated, preferably by promoting teamwork, where every individual is well aware of their individual and corporate responsibilities through a formal assignment of duties.
Medical ALARA Culture must fit in with, and be complementary to medical practice rather than being regarded as an external requirement.
We have presented arguments that support radiation protection and a Medical ALARA Culture to mitigate against the risks from the use of ionising radiation in healthcare. However, it should be remembered that a Medical ALARA Culture is part of the wider safety culture in the healthcare environment and an Integrated Risk Management System can be key for a successful healthcare Quality Management System.
References
[1] OSHA, Categories of potential hazards found in a hospital, available at: http://www.osha.gov/SLTC/healthcarefacilities/hazards.html, as accessed on the 22nd of August 2010.
[2] Graham, A., Integrated Risk Management Implementation Guide, available at: http://post.queensu.ca/~grahama/publications/TEXTPDF.pdf, as accessed on the 22nd of August 2010.
[3] Schmitt-Hannig, A., EAN Working Group on ALARA Culture, European ALARA Network, available at: http://www.eu-alara.net/index.php?option=com_content&task=blogsection&id=9&Itemid=119, as accessed on the 22nd of August 2010.
[4] EAN, EAN proposal: Definition of the ALARA Approach to Radiation Protection Culture, available at: http://www.eu-alara.net, as accessed on the 22nd of August 2010.
[5] European Commission, Council Directive 96/29/Euratom of 13 May 1996 laying down basic safety standards for the protection of the health of workers and the general public against the dangers arising form ionising radiation, OJ L159, 29.6.1996, p. 1114.
[6] European Commission, Council Directive 97/43/Euratom of 30 June 1997 on health protection of individuals against the dangers of ionising radiation in relation to medical exposure, and repealing Directive 84/466/Euratom, OJ L180, 9.7.1997, p. 22-27.
[7] European Commission, Radiation Protection 118, Referral guidelines for imaging, Directorate-General for the Environment, 2000.
[8] SHIMIZU, Y., KODAMA, K., NISHI, et al, Radiation exposure and circulatory disease risk: Hiroshima and Nagasaki atomic bomb survivor data, 1950-2003, BMJ. (Jan. 2010).
[9] SMITH-BINDMAN, R., LIPSON, J., MARCUS, et al., Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer, Arch. Intern. Med. 169 22 (Dec. 2009) 2078-2086.
[10] MULLENDERS, L., ATKINSON, M., PARETZKE, H., et al, Assessing cancer risks of low-dose radiation, Nat. Rev. Cancer 9 8 (Aug. 2009) 596-604.
[11] Uffman M., Shaefer-Procop C., Digital radiography: The balance between image quality and required radiation dose, European Journal of Radiology 72 (2009) 202-208.
[12] CIRAJ-BJELAC, O., REHANI, M.M., SIM, K.H., et al, Risk for radiation induced cataract for staff in interventional cardiology: Is there reason for concern? Catheter. Cardiovasc. Interv. (Jun. 2010).
The 3rd EANNORM workshop was held from 23 - 25 November 2010 in Dresden, Germany. It was organised and hosted by IAF - Radioökologie GmbH and supported by the Federal Office for Radiation Protection Germany. This workshop was dedicated to the topic Scenarios for Dose Assessments in the NORM industry". Its main goal was to familiarise the participants with different approaches developed for dose calculations in the NORM industry and to discuss the question as to whether a harmonization of these approaches should be pursued or not. Forty five experts, coming from 14 countries, took part in the discussions and shared their experiences.
Each speaker was allocated 45 minutes which included ample time for discussion. Each daily session was followed by a special round table discussion of about one hour on "burning questions". The talks reflected a wide range of situations in which the presence of NORM can cause radiation exposures to workers and/or to members of the public at a level which cannot be ignored from the radiation protection point of view. The scientific program and the single presentations of the EANNORM Round Table Workshop on Scenarios for Dose Assessments in the NORM industry" are available at the EANNORM web-page www.ean-norm.net.

The main conclusions of the EANNORM Round Table Workshop on Scenarios for Dose Assessments in the NORM industry" were:
- We are still some way from a harmonisation of methods suited for dose assessment in the NORM industry.
- We need European guidelines for the measurements of key parameters for dose assessment and calculation of the dose for workers and, if necessary, for members of the public, too.
- The Calculation Bases for the Determination of Radiation Exposure due to Mining-caused Environmental Radioactivity (Calculation Bases Mining) published by the Federal Office for Radiation Protection (Germany) could be a basis for such a guideline.
- Measurements of the ambient gamma dose rate are one of the principal components of the monitoring programmes for workers in the NORM industry. Therefore, measurements have to be justified, since they are not applicable for a wide range of NORM.
- Radon that is released from raw materials processed in the NORM industry or from industrial residues can dominate the total exposure of persons at work. A method should be developed in order to assess the contribution of radon released from the materials of concern to the indoor concentration. The method should also be suitable to assess the release of radon from the building materials to the indoor concentration in dwellings.
- The specific activity of NORM is the basis for several assessments and therefore a key parameter in the radiation protection practice. How should it be measured efficiently and reliably, taking into account the variety of materials?
- Some of the most commonly discussed topics within the network include cross border material handling and transport of NORM in the context of different national positions. However it was agreed that the problem can only be solved in a political framework and the EC should come to a commonly accepted solution as soon as possible.
- The present state and the future of the EANNORM was the subject of a lively discussion. In particular, the participants recognised the advantages of having a well-working network with members coming from all European states as well as from abroad. The website currently gets about 1000 daily visits from members and non members of the EAN-NORM. However the fate of the network depends on the future financing.
1 Physikalisch-Technische Bundesanstalt, Braunschweig, Germany
2 Bundesamt für Strahlenschutz, Berlin, Germany
Abstract
The German X-ray Ordinance lays down the basic requirements for type approvals of X-ray devices. In Germany, type approvals according to the Radiation Protection Ordinance and the X-ray Ordinance are issued by the Federal Office for Radiation Protection (Bundesamt für Strahlenschutz, BfS). The type testing of X-ray devices is carried out by the Physikalisch-Technische Bundesanstalt (PTB), the German National Metrology Institute and the highest technical authority of the Federal Republic of Germany for the field of metrology and certain sectors of safety engineering. In 2010, a new X-ray Ordinance is to come into force in Germany. This ordinance will introduce a new category of type-approved X-ray devices, called basic-protection devices, in addition to the existing five categories. In general, type approvals shall ensure high safety standards in radiation protection. In particular, the exposure of operators due to ionising radiation shall be kept as low as reasonably achievable (ALARA principle).
In the following sections, the technical requirements for basic-protection devices as well as the type-test procedures for this new category of X-ray devices will be outlined.
1. Introduction
The basic safety standards for the protection of the health of workers and the general public against the dangers arising from ionising radiation are laid down by European Council Directive 96/29/EURATOM [1]. This Directive applies to all practices which involve a risk from ionising radiation, namely (according to article 2):
- (a) the production, processing, handling, use, holding, storage, transport, import to and export from the European Community and the disposal of radioactive substances;
- (b) the operation of any electrical equipment emitting ionising radiation and containing components operating at a potential difference of more than 5 kV;
- (c) any other practice specified by the Member State.
In Germany, these basic standards are implemented through the Radiation Protection Ordinance [2] (the current version came into force in 2001) and the X-ray Ordinance [3] (considerably amended in 2002). The Radiation Protection Ordinance (Strahlenschutz-Verordnung) provides regulations for the handling, use, storage, transport and disposal of devices containing radioactive substances. In addition, this ordinance governs the operation of accelerators or X-ray devices with high voltages exceeding 1 MV, whereas the X-ray Ordinance (Röntgen-Verordnung) provides regulations for the operation of X-ray devices with acceleration voltages between 5 kV and 1 MV and the operation of sources of stray radiation.
In general, an authorisation by the local supervisory authority is needed for practices which involve a risk from ionising radiation emanating from an artificial source. However, practices regulated by the German Radiation Protection Ordinance do not require an authorisation nor reporting, when a type-approved device is operated. On the contrary, according to the German X-ray Ordinance, the operation of type-approved X-ray devices in general requires reporting to the responsible authority. For that reason, the 1 µSv h-1 concept of Article 3 No. 2 of Council Directive 96/29/EURATOM is not applicable in Germany, as far as X-ray devices are concerned. As a consequence, the dose rate limits defined by the German X-ray Ordinance differ considerably from 1 µSv h-1 and vary strongly with the kind of X-ray device and its application. A more detailed description of the various categories of type-approved X-ray devices, as defined by the German X-ray Ordinance, follows below.
2. Type approvals in Germany
BfS is responsible for issuing German type approvals according to the Radiation Protection Ordinance and the X-ray Ordinance. In accordance with these ordinances, prior to issuing a type approval BfS initiates a type test by PTB. Concerning devices containing an encapsulated radioactive source a further technical authority, the Federal Institute for Materials Research and Testing (Bundesanstalt für Materialforschung und -prüfung, BAM), is involved in issues concerning leakage, materials chosen and the design of the encapsulation of the radioactive substance and quality assurance. Both ordinances mentioned do not constitute a claim for type approvals. This means that only devices or X-ray tube assemblies which assure a high safety standard according to the state of the technology can get a type approval.
2.1 Type testing of X-ray devices
The amended version of the German X-ray Ordinance of 2002 distinguishes between the following categories of type-approved X-ray devices:
- X-ray tube assemblies (Röntgenstrahler) - Combinations of an X-ray tube with a protective tube housing. In some cases, the high voltage (HV) generator is included in the housing.
- High-protection devices (Hochschutzgeräte) - X-ray devices which completely enclose the sample to be investigated, with the exception of small openings which allow only a hand to be entered.
- Full-protection devices (Vollschutzgeräte) - X-ray devices which can be operated only when the sample to be investigated is completely enclosed by the protective housing. This has to be safeguarded by two independent safety circuits.
- School X-ray devices (Schulröntgeneinrichtungen) - Full-protection devices with additional safety requirements. They are used for educational purposes in schools.
A new category of X-ray devices called basic-protection devices will be implemented by the forthcoming amended version of the X-ray Ordinance, which is expected to come into force in 2010:
- Basic-protection devices (Basisschutzgeräte) - This new category will comprise cabinet X-ray systems which fulfil special requirements described below in section 2.3.
Table 1. Dose rate limits for type-approved X-ray devices and sources of stray radiation
| Category of type-approved system | Dose rate limits at the specified distance | Distance | |
| According to current X-ray Ordinance [2] | According to X-ray ordinance of 2010 | ||
| X-ray tube assemblies | 2.5 mSv.h-1 (V ≤ 200 kV) | 2.5 mSv.h-1 (V ≤ 200 kV) 10 mSv.h-1 (V > 200 kV) | 1 m from the focal point |
| Basic-protection devices | n/A | 10 µSv.h-1 | 0.1 m from any accessible surface |
| High-protection devices | 25 µSv.h-1 | 10 µSv.h-1 | 0.1 m from any accessible surface |
| Full-protection devices | 7.5 µSv.h-1 | 3 µSv.h-1 | 0.1 m from any accessible surface |
| Sources of stray radiation | 1 µSv.h-1 | 1 µSv.h-1 | 0.1 m from any accessible surface |
Table 2. Organisational requirements for the operation of type-approved X-ray devices and sources of stray radiation
| Category of type-approved system | Report of authorised expert prior to start-up | Local radiation protection regime | Report of authorised expert every 5 years |
| X-ray tube assemblies | X | X | X |
| Basic-protection devices | - | X | X |
| High-protection devices | - | X | X |
| Full-protection devices | - | - | X |
| Sources of stray radiation | - | - | - |
Full-protection devices are the only kind of type-approved X-ray devices which may, after prior reporting to the local authorities, be operated without having a pronounced radiation protection regime (i.e. without being investigated by an authorised expert prior to start-up, without the supervision of a radiation protection officer during the operation and without requiring any technical or radiation protection qualifications of the operator). Therefore, high technical safety standards have to be fulfilled in order to achieve a type approval for full-protection devices.
2.2 Technical requirements for type-approved devices
According to the X-ray Ordinance, high-protection devices, full-protection devices and school X-ray devices must meet the requirement that the X-ray tube or the X-ray tube assembly can only be operated if the protective casing is completely closed, which for the latter categories must be guaranteed by two independent safety circuits (exceptions are regulated in Annex 2 to the X-ray Ordinance). Detailed technical specifications regarding the implementation of this requirement have been established by a decision of the German Federal States of March 28, 2002:
- The safety protection system used must comply with the safety degree of "category 3" specified in standard EN 954-1 [4]. In addition, the relevant regulations of standard DIN 54 113, part 2, are to be met [5]. This ensures that the failure of a component is detected at the latest when the operator tries to restart the device, so that the switching-on of the X-ray tube is electronically prevented.
- Full-protection devices, school X-ray devices and high-protection devices must be provided with a time-delay function so that opening of the casing will be possible only if the acceleration voltage of the X-ray tube is less than 5 kV.
2.3 Technical requirements for the new type Basic-protection devices
Frequently, automatic X-ray scanners are used in industry and in safety applications for a variety of purposes: analysing the composition of food or technical materials, checking packages for foreign objects, checking the correct filling of non-transparent packages or cans, inspecting luggage for illicit items, just to list some examples. These systems are typically used in automated production lines of for example the solid-state industry, the food industry and during luggage inspections at airports or other facilities. A type test of the included X-ray tube on its own is not appropriate, because this test would merely guarantee, that the ambient dose equivalent rate at 1 m from the focal point of the tube would be lower than 2.5 mSv h-1 or 10 mSv h-1, depending on the operating voltage. This value is much too high if personnel or members of the public stay close to an X-ray scanner, as is typically the case for luggage inspection devices. An adequate category was, however, not defined in the X-ray Ordinance, so that these scanners could not be type tested appropriately in the past. Thus, a new category, named "Basic-protection devices", had to be defined.
What are the common characteristics of basic-protection devices? For practical reasons, the protective casing of this type of device cannot be completely closed. Usually, the protective casing has two apertures connected to a transport system; one for the insertion of goods and another for the removal of goods after they have been inspected. The apertures are sometimes covered by a flexible protective curtain to limit leakage radiation. The automatic transportation systems for the inspected goods are a protection against unwanted irradiation of human beings, but in some cases cannot prevent people from entering a transport belt completely. Therefore, the protective level of these kinds of devices is lower than that of full-protection or high-protection devices.
The following requirements for basic-protection devices will be introduced:
- It has to be ensured that the protective casing encloses the X-ray tube and the object to be examined completely while the X-ray tube is in operation. Apertures are merely admissible for the automatic transportation of inspected goods and their dimensions have to be adapted to that purpose.
- The dose rate limits for type-approved basic-protection devices at a distance of 0.1 m from the surface of the protective casing and at a distance of 0.1 m from the apertures may not exceed 10 µSv h-1 under maximum operating conditions.
- If a continuous operation of the X-ray emitter is required, its operation without completely closed protective casing is allowed only if the dose rate inside the protective casing does not exceed 10 µSvh-1.
3. Summary and conclusions
In Germany, type testing and type approvals are an important basis for the high safety standards, that protect workers and members of the public against avoidable exposures to ionising radiation. Certain categories of devices or apparatus are defined by law. This categorisation system defines different safety levels with increasing technical requirements, in order to allow for a stepwise reduction of organisational radiation protection. Therefore, type approvals help:
- to keep the exposure from X-ray devices under normal operation conditions to human beings "as low as reasonably achievable" (ALARA),
- to minimise the risk of failure that may cause harmful exposures, by state-of-the-art technical means and
- to minimise the administrative expenditure for operators of X-ray devices and authorities (no individual authorisation for type-approved devices needed).
References
[1] European Commission, Basic safety standards for the protection of the health of workers and the general public against the dangers arising from ionizing radiation, Council Directive 96/29/EURATOM of 13 May 1996, Official Journal of the EC L159, Vol. 39 (Luxembourg: Office for Official Publications of the European Communities) (1996).
[2] Verordnung über den Schutz vor Schäden durch ionisierende Strahlen (Radiation Protection Ordinance - Strahlenschutzverordnung - StrlSchV) of 20 July 2001, BGBl. I S. 1714, latest revision on 13 December 2007, BGBl. I S. 2930 (2007).
[3] Verordnung über den Schutz vor Schäden durch Röntgenstrahlen (X-ray Ordinance - Röntgenverordnung - RöV) of 8 January 1987, published as amended on 30 April 2003, BGBl. I S. 604 (2003).
[4] European Committee for Standardization (CEN), Safety of machinery Safety-related parts of control (EN 951-1:1997-03) (Brussels: CEN) (1997).
[5] Deutsches Institut für Normung (DIN), Non-destructive testing- Radiation protection rules for the technical application of X-ray equipment up to 1 MV (DIN 54113-1 to -3) (Berlin: DIN) (2005).
